-
January 12, 2026: Kinky bitch!
Fast facts (if you don’t have time to read the full post): New year, same medical nightmares. Except I am now another year in and another year wiser. We started 2026 off strong with an MRI of my lower back due to a cry for help I made to my onco in December (hello horrific back pain!) And somehow, that was the least of my worries during the first week of January. Lord Voldeport took over the spotlight, not giving blood two days in a row and I once again left the cancer center in a fit of tears. I am just going to say it now: this needs to be a year where I am not suffering from constant medical trauma.
TO THE LONG VERSION!
For as publicly as I have chronicled my cancer journey, I feel myself pulling inward now, afraid of being too much, of being seen as overdramatic, because there is always something going on with me medically. For a journey I once believed would have an end, it turns out at least for me there isn’t one.
Instead of posting stories about appointments going sideways or the weird new things I’m learning about my body, I’ve chosen to swallow them whole. In turn, it’s made me mentally sick. I often leave appointments in tears, unsure where to place the burden of my chronic illness when it feels too heavy to share with anyone but myself. Once a month, I purge it all in therapy… and then I start the cycle again.
I’m trying to be better about sharing, at least informing the people closest to me about what’s going on with my care, but I’m exhausted. And I know everyone else is, too.
I’m not saying my support system is exhausted because of me. But medical fatigue is real, and in a world that already feels crushing—politically, socially, existentially—sometimes people just don’t have spoons to give. I understand that. I grieve alongside everyone else. It’s hard to care deeply about anything when everything feels like it’s on fire.
In September, I shared about my surprise surgery for a new port, a decision I didn’t make lightly. There were people in my support circle who didn’t understand why I would choose another surgery, another device implanted in my body. But the mental gymnastics of peripheral blood draws and the “will Harry Porter or won’t Harry Porter give blood today” had become more than I could handle.
The first couple of draws went semi smoothly. I could finally breathe. And then… December happened.
I’m nonconfrontational by nature, but I’ve made it my personal mission to be better at saying how I feel, especially when it comes to my medical care. Self-advocacy is one of our greatest superpowers, but it takes time, education, research, introspection, and knowing your rights as a patient. None of that comes naturally when you’re exhausted, scared, or just trying to survive.
I was supposed to have my monthly set of appointments on Christmas Eve. Two days before, I found myself sick with the flu. I called and canceled, and was told, No worries! See ya next year!
SIKE!
Christmas Eve, my phone rang. It was the cancer center. My oncologist wanted me to come in that Friday for my injection but said I could skip labs.
“But I’m sick with the flu,” I said. “I should be fever-free by Friday, but I probably still won’t feel great.”
“Wear a mask,” they said.
Uh. Okay?
So I made my way down to the cancer center for my monthly stabbing and left with my prized Tillamook cheese. Things are going to be okay, I told myself. (They were, in fact, not okay.)
The following Monday, I got a call from Priscilla, one of my favorite medical assistants and who I liken to my personal liaison with my oncologist’s office and staff. My oncologist wanted me to come in for my quarterly ctDNA blood draw.
“But I was just there on Friday,” I said.
We talked at length about how I’d just been there, how I’d be back in three weeks anyway, how often I’m already at the cancer center: once a month for labs, a provider visit, and an injection, and then sometimes another separate visit just for ctDNA. I complained about how it takes me away from living my life, from being at work, and how I didn’t understand why these labs couldn’t be combined.
“Tell my oncologist I’m not coming in,” I said, suddenly very brave. “We can do it in a couple of weeks.”
She agreed. I hung up feeling like I’d won.
Wrong.
On Monday, January 6, she called me back. “Z wants you in this week. I am so sorry.”
The rage I felt in that moment was cartoonish. I was seeing red. Steam out of my ears. Full Looney Tunes meltdown. I was too tired to fight and made the appointment for Wednesday at 7:30 am and hung up.
Meanwhile, I was also trying to psych myself up for an MRI scheduled for later that night because why have one emotionally destabilizing medical event when you can have two?!
Sometime after Thanksgiving, I started experiencing intense back pain. Sometimes it was in my lower back, sometimes between my shoulder blades, sometimes shooting straight down my spine. For several nights in a row, the pain was so intense I couldn’t sleep. When I was first diagnosed in 2022, my metastatic lesions didn’t cause pain, so I had no idea what to make of it.
I let it go on for two and a half weeks before finally calling triage. Either this was a fucked-up back injury or it was cancer. I just need to rule out the cancer.
To my surprise, my oncologist agreed to order imaging. I was disappointed there were no open appointments in December. I’d already met my out-of-pocket max, and the idea of waiting weeks for answers felt cruel. But as time passed, I noticed improvement. Stretching helped. Physical therapy helped. Massage helped. Modifying CrossFit workouts helped.
Maybe it wasn’t cancer. But then what was it???
I was sitting at the kitchen table eating dinner with my roommate when my phone rang.
“If you’re able to come in sooner, we have availability right now.”
“Oh cool,” I said. “I could be there in about 30 minutes. I’m just about to put lidocaine cream on my port.”
“Your port? We can’t access that tonight. Nurses go home at four. We’d have to use your arm.”
Panic. Immediate panic.
If I went in, I’d be reliving the mental torture of my first MRI with my first cancer-related needle experience. If I rescheduled, when would I get back in? I’d already waited weeks.
“That won’t work for me,” I said. “I’m a hard poke and I have a port. When can I reschedule?”
“How about tomorrow at 3:30 pm?”
I hadn’t realized how much air I was holding until I exhaled. I accepted immediately.
The next day was gloomy as I zipped across town to the hospital. I checked in, sat down, and started casually circling answers on my paperwork when a man yelled my name across the lobby.
“Hi, I’m Travis. Let’s go do your MRI.”
Here’s the thing, Travis. I have terrible memory recall for important things—birthdays, names, passwords—but my brain is excellent at remembering trauma. And as soon as I heard his voice, I knew.
You’re the guy.
You did my MRI four years ago.
You’re my grim reaper, dude.That’s what I wanted to say.
Instead, Anxious Madison took the wheel and started oversharing about every piece of metal in my body: my tragus piercing I can’t remove, the permanent bar behind my front teeth. Travis was not impressed, nor interested in making me feel better. I basically talked into the void as we walked down the creepy hallway.
After escorting me to the room to change into more MRI-friendly clothes, I sat on the oversized chair waiting for the nurse to access my port. She was not a beacon of comfort. As she prepped her materials, I looked across the room and saw four men in scrubs, including fucking Travis, yapping and telling jokes. It felt like a frat house somehow sandwiched between two MRI machines.
The nurse pushed me back into the chair, stretched the skin around my port with two fingers, and inserted the needle. The aggression of the insert caught me off guard. It was not a sensation I was familiar with. She flushed the port and asked, “Is it normal for you not to have blood return?”
“This is a new port,” I said. “It should be in perfect working order.”
Sure enough, blood appeared briefly, and I was whisked off to the land of doom.
Travis robotically instructed me on where to lie down and asked what kind of music I wanted to not hear through the headphones.
“EDM, please,” I said.
He slid the headphones over my ears, placed something over my arms and hands, and pressed a button to slowly send me into the machine.
“This okay for you?” he asked, pointlessly.
Yeah, Travis. Being forced into a magnet tunnel is exactly how I wanted to skip work today.
I nodded. He handed me the panic squeeze-ball and stepped away. And once again, just a month shy of four years later, I was alone with the violent beeping of the machine, my spiraling thoughts, and Rihanna whisper-singing, “Please don’t stop the music.”
The amount of times I had to tell myself not to move was honestly hilarious. Have you ever laid so still that you become convinced you’re moving? The sudden itches were out of control. My body was deeply offended by the request to remain motionless, and the thirty minutes in the tunnel of doom felt like an eternity.
But all scans, thankfully, do come to an end. Before I knew it, Travis was helping me out of the machine. I sauntered back to the oversized chair and waited for the nurse to return and de-access me, bracing myself for whatever came next.

~MRI fit~ “Okay, one, two, three,” she said, and aggressively yanked the needle out. I turned my face to the side from the force and heard the device clatter loudly into the plastic trash can.
“Oh! You’re bleeding all over,” she exclaimed.
I looked down to see a trail of blood from my port, gathering into a little pool and soaking inside of my white camisole.
“I didn’t know you were a bleeder,” she said, genuinely shocked.
Me either, lady.
I raced back to work, still buzzing, still sore, still smelling faintly like antiseptic, only to be greeted an hour later by a new notification in MyChart.
MRI results already???
I opened them and learned that three of my four metastatic lesions were completely resolved. No new lesions were seen in the area. I also apparently have a disc bulge, which has made appearances on other scans and neatly explains my back pain.
Objectively, this was very good news. Incredible news, even.
But that relief was quickly overshadowed by my inability to understand what was written about the fourth lesion:
Vertebrae and vertebral marrow signal: No acute fracture is
demonstrated. There is a small area of reduced signal intensity on T1
imaging measuring 13 x 9 mm within the L1 vertebral body on image 6 of
series 3 previously measuring 9 x 12 mm. There is progressive fatty
metaplasia of the marrow at L1 which may reflect post radiation
changes. This lesion reveals no significant enhancement. Previously
noted enhancing lesions at L3, L4 and L5 are resolved. No new
enhancing lesions are seen of the lumbar spine.Anxious Madison clocked in immediately. My heart was jumping in my ears as I reread the report over and over, trying to make sense of it. You say there’s a lesion with reduced signal intensity, but then you say there’s no significant enhancement. And then I initially read it as being on my T1 instead of my L1 which, for those unfamiliar with spines, is much higher, and I was baffled because I thought all my lesions were in my lower back.
So, naturally, I spiraled.
Later that evening, a few friends graciously read the report for me and confirmed what my anxious brain could not: the lesion is in my L1, the report is just written weird, the lesion is inactive, and I am still no evidence of active disease.
I wish I could take the win. I wish I could celebrate the fact that THREE OF MY FOUR LESIONS ARE FUCKING GONE.
But no. I had barely come down one mountain before I was already climbing another: an unnecessary port draw.
Day 1 at the Cancer Center –
Wednesday morning came fast. I arrived early, optimistic, cheerful even. I’d seen blood return the day before during my MRI, so I felt confident. I’d be in and out, no problem, and then off to get myself a lil treat as a reward before work.
That confidence faded quickly.
After her second flush, nurse Megan began pumping for blood return.
“I literally had blood return yesterday,” I offered, politely panicking.
For thirty-five minutes, we worked my port. I did squats. I walked in circles. I did elephant breathing. I turned my head in every direction like a possessed owl. Lord Voldeport refused to give up the goods.
“I need to go to work,” I finally said, defeated. It was almost nine, so this would mean no treat for me.
We de-accessed with the plan for me to return the next afternoon.
On my way out, I stopped to chat with a few nurses and Priscilla. Back in November, I’d asked her to see if my oncologist would order a blood type test because I am four years deep into this nonsense and still have no idea what type of blood is inside of me!
“So… bad news,” she said. “Z denied your request.”
I wonder if my eyes looked like daggers.
“Seriously?” I said, doing my best to restrain my rage.
I understand it’s not a necessary test. But if I’m already having blood drawn, and I’m happy to pay for it, I don’t see the harm. Maybe insurance needs justification, sure, but it felt like just another reminder that I have very little agency over my own body or really any of the testing.
“If we can get my port to work,” I asked before leaving, “can you also ask Z if we can do my other labs so I don’t have to do this again in two weeks? This is just too much.”
“I’ll see what I can do,” she said.
Day 2 at the Cancer Center –
I intentionally scheduled my next blood draw for 3:30 pm. That way I would’ve already gone to the gym, moved my body, drank a shit ton of water, and eaten. I consider these the holy trinity of port success.
I sauntered into the lab, once again ready for the assault on my chest.
And once again déjà vu.
We lined up the vials for my sacrificial offerings, flushed my port several times, and watched… nothing. Not even a tinge of blood. Forty-five minutes later, the nurses decided to send me to the chemo pods for tPA.
“This is going to work,” nurse Hanane assured me as she injected the medication. “Your port is new. It’ll work like a dream.”
I left thirty minutes later with a bruised ego, a chunk of cheese, and a very sore accessed port.
Day 3 at the Cancer Center –
If you’ve ever slept with your port accessed overnight, you know my pain. My chest was tight and sore when I woke up. I slept like shit because sleeping with a needle in you is not comfortable, and I couldn’t shake the thought that if I turned just right, the needle would somehow escape and stab me somewhere else, and I’d slowly bleed internally.
Sounds like a great episode of “House.”
I went to CrossFit before my blood draw, thinking tPA plus exercise would seal the deal. Working out with a needle in your chest is deeply awkward. I didn’t want to accidentally hit it with a barbell, and I don’t enjoy drawing attention to my chest, but my port was very much on display.
Workout done, I drove across the street to the cancer center, hoping this would be the last time I’d be there that week. As much as I love seeing my friends, every appointment feels like the start of a new trauma I’ll need several therapy sessions to unpack.
I plopped into the chair and watched as Rachel flushed my port. Blood slowly filled the discard vial.
“Oh fuck,” I said. “I am so happy.”
And maybe I should have shut the fuck up.
One vial into the seven I needed, my blood stopped moving.
“I’m scared to flush you because it might go away,” Rachel admitted.
But I had to be flushed. And sure enough, the blood return stopped.
Tears welled immediately.
I began the ritual again: coughing, massaging my neck, squatting, bending over. Panic crept in. Nurse Jessie appeared and joined us. After a few more minutes, she suggested I try laying down.
In another room, I reclined while Rachel continued working on my port and Jessie examined my chest, massaging around it.
“This feels weird,” Jessie said. “Does this hurt?” she asked, pressing along the noodle part of the port tubing.
“No, just really weird,” I said, as tears slipped down my face. I was already preparing myself for a peripheral draw.
Jessie kept massaging, then suddenly paused.
“Don’t move,” she said. “I think your port was kinked. I just unkinked it and you’re giving blood.”
The tears came faster; relief tangled with distress. Lord Voldeport isn’t even four months old and this little bitch is already fucking kinked. But suddenly everything made sense: why I could flush perfectly but get nothing in return, and why there’s been a weird little bump in my neck this whole time.
Epilogue
All of this happened in the span of four days.
Four days of living on the edge of my seat, unable to relax, waiting for the next call, the next appointment, the next thing to go wrong. I missed more work than I wanted to. And when I was at work, I wasn’t really there. I was being pulled away physically by appointments and mentally by the world I kept getting dragged back into.
That’s the part people don’t always see: you can leave the cancer center, but the cancer center doesn’t always leave you.
By the end of it all, everything technically worked out. My labs were eventually drawn. My port is kinked but not broken (so now we know what to do for my next draw!) My MRI showed good news. Nothing catastrophic happened. And yet the amount of strife this caused me, mentally and physically, was enormous. It was draining in a way that doesn’t show up on scans or lab reports.
In two weeks, I’ll be back again. I won’t even see my oncologist, just one of the ARNPs. And somehow I need to figure out how to explain how distressing all of this is, while also acknowledging that my cancer center appointments are not the only things on my schedule. There’s physical therapy. Massage therapy. Regular therapy. Sometimes all three in the same week, like a deranged wellness bingo card. I rarely go a full week without at least one appointment. At this point, I’ve joked that the cancer center should give me a punch card: ten visits and the eleventh is free, or maybe the prize is just a sticker that says “Congratulations! You’re not dead.” All of this, every appointment, every punch, every calendar alert, is in the name of keeping me alive, keeping me functional, and trying to rebuild a body that has been through more than one person should reasonably be asked to endure. It’s healthcare, yes. But it’s also a constant reminder that being alive like this means being a lot: a lot of appointments, a lot of effort, a lot of me.
I know this could have been worse. I know that. Compared to how January started last year with a DVT, this is just some bullshit I can sort out. A disc bulge isn’t great, but it’s a hell of a lot better than metastasis. I am grateful. Truly.
But also? I am so fucking tired of having fucked up things happen to me.
This is the part I usually swallow whole. The part I convince myself is too heavy, too repetitive, too much. Not the gratitude, not the resilience, but the exhaustion. The quiet accumulation of stress that never fully leaves my body.
Maybe writing this down is me setting it down instead of carrying it alone.
I don’t need miracles.
I don’t need dramatic wins.I just need the sun to shine on me for a bit.
2026. Still here. Still in it.
Today’s song lyrics of the day are brought to you by Armin van Buuren.
“If you need a hero
I guess I’m not that guy
I’m running with the mile high club and we’re fucking in the sky
I’m just hoping that the sunshine shines on me
On me” -
Living in the Paradox
Prologue –
This year has been heavy. The kind of heavy that seeps into your bones and sits there, unmovable. Too many women I’ve known through metastatic breast cancer are gone now, and their absence lingers like a shadow. I keep wondering when my story might start to sound more like theirs.
I live with stage IV breast cancer: a disease that is treatable but not curable. That means my life exists in the space between miracle and uncertainty. Between gratitude and rage. Between the urge to hope and the ache of knowing too much.
Living with metastatic breast cancer is a constant balancing act between scans and side effects, between wanting more time and fearing how little there might be. But it’s also a call to action. Because awareness without understanding isn’t enough. Because pink ribbons don’t tell the whole story. Because only a small fraction of research funding is dedicated to the very disease that takes the most lives.
So as you move through this month of pink, I ask you to look deeper. Learn what metastatic breast cancer really means. Support research that focuses on extending lives (METAvivor is a great place to donate to!), not just catching disease early. See the people living with it not as symbols of survivorship, but as whole humans navigating both hope and heartbreak.
The words that follow were written from that space. From a body that keeps going, even when it hurts. From a heart that speaks not for sympathy, but for change.
The following piece was originally published in Tumbleweird’s October 2025 edition.
When I was diagnosed with metastatic breast cancer, one of the first things someone said to me was, “Oh, you’re so young! At least you’ll bounce back faster.” As if youth were a cancer repellent — SPF for rogue cells.
That phrase, “At least”, kept showing up, in every flavor — sympathy, awe, relief.
“At least it wasn’t worse!” As if stage IV wasn’t the worst it could be before dying.
“At least it’ll grow back!” As if losing your hair (and your eyebrows, and your lashes) isn’t a big deal.
“At least you have support!” As if I didn’t watch people exit one-by-
one from my life, unable to bear the emotional load of my illness.“At least you’re alive!” As if I should send cancer a thank you card for not
killing me… yet.The thing about “at least” is, it’s intended as a life raft, a way to keep you afloat while cancer threatens to pull you under, a way to keep you from drowning in fear and uncertainty. More often, though, it feels like slapping a Post-it note over a gaping wound: “There! Fixed it!”
The “at leasts” pile up, and you start feeling like you’re expected to be the mascot of gratitude — always smiling and positive, just happy to be alive! Never mind that your body feels like a junk drawer full of broken parts, you put on the mask, say “Yes, thank you. At least there is that,” and hope no
one notices the cracks in your grin.The thing about masks is: you wear them too long, you suffocate.
Make no mistake! I am deeply, fiercely, desperately grateful to still be here. I feel it when I watch little birds eat the sunflowers in my front yard, when I bake endless loaves of focaccia for my friends, when I quench my skin in
unexpected rain. But gratitude does not cancel out grief. It is not morphine.
It does not ease the aching bones, or quell the hot flashes. It does not return my sovereignty over my body, or erase the surgery scars.Gratitude does not change the dire truth: One day, this disease will likely kill me.
Sometimes gratitude is a mask I wear so the world doesn’t run screaming from my reality.
The reality of cancer is messy. It’s ugly-crying in the shower when you realize you’ll never breastfeed children you don’t even have. It’s joints creaking like a haunted farmhouse, at the ripe old age of 33. It’s choking down yet another chalky, despair-flavored pill and calling it ‘treatment’. It’s mapping your life around scan days and monthly blood draws, and being paralyzed by anxiety for the following 24 hours waiting for results.
If I admit any of this out loud, I feel the silent judgment: Is she grateful
enough? As if survival comes with a gratitude quota.I am grateful, but I am also angry.
I am grateful, but I am also tired.
I am grateful, but I am also scared.These things cohabit in my chest like roommates arguing over thermostat settings, and honestly, some days, the rage shouts louder than my gratitude.
I’m angry at the time cancer has stolen from me, that my body most likely cannot give me children. I’m angry that my body is both a miracle of survival and a ticking time bomb. I’m angry that my vocabulary includes things like ‘neutropenia’ and ‘osteonecrosis of the jaw’ when I should be stumbling through the pronunciation of obscure wines on a bar menu.
However, rage may own the apartment, but life is not easy to evict.
The woman who screams in her car after a stomach injection also sings on the freeway home. The body that aches with side effects also dances barefoot in the kitchen. The heart which fears recurrence never stops wanting more, even when wanting feels dangerous.
The cruelest part of “at least” is the implication that those living with cancer should be content with survival; that we should not grieve what cancer took because we are, after all, still here.
But I do grieve. I will always grieve. And that grief does not cancel my gratitude.
This month, pink ribbons will adorn storefronts and social media posts, and the word “awareness” will scatter through the air like confetti. However, October 13, Metastatic Breast Cancer Awareness Day, doesn’t get the same spotlight, despite the fact that survivorship isn’t guaranteed.
Stage IV isn’t the ‘bad luck’ exception. It’s the lived reality of too many of us — early detection saves some lives, but it doesn’t save every life.
Metastatic breast cancer is initially located in the breast before metastasizing (spreading) to other areas of the body. According to the Breast Cancer Research Foundation: Metastasis occurs when breast cancer cells break away from the original tumor or nearby lymph nodes (found under the arm, inside the breast, and near the collarbone). The breast tumor cells then enter the bloodstream or lymphatic system, travel to other organs, and begin to grow. Doctors most commonly find metastatic breast cancer in the bones, lungs, liver, and / or brain.
Metastatic breast cancer is a paradox: treatable (for some) but incurable— somewhat survivable without survivorship. As of 2025, an estimated 200,000 women in the U.S. are living with metastatic breast cancer (JNCI Cancer Spectrum: Volume 5, Issue 4). The five-year survival rate is only 31.9%. Despite these numbers, only 3–5% of research funding is dedicated to understanding stage IV disease, how metastasis happens, and how to save the people living with it.
Even those numbers don’t fully explain the paradox of living with metastatic breast cancer, and here’s what I wish I could say out loud:
I wish cancer had never touched me.
I wish I didn’t know what it feels like to live in a body that betrayed me.
I wish I didn’t spend every scan day rehearsing how to hold my breath.
I wish I could say “everything happens for a reason” and believe it.The truth is, sometimes, life is just fucked. My gratitude coexists with
rage. My love coexists with grief. My hope coexists with fear. None of those
things cancel each other out and no “at least” statement can make me
pretend otherwise. So if you hear me say, “I’m fine” or “I feel lucky” or “I’m grateful”, know that those words are true, but they’re not the whole story.Sometimes gratitude is a mask. Sometimes it’s armor. Sometimes it’s the thing I say to make both of us feel better.
Underneath it all, I am a woman learning to live in the paradox: thriving and grieving at the same time.
-
September 28: Endless summer
Fast facts (if you don’t have time to read the full post): My two months away from work has sadly come to an end. I return to my mundane routine tomorrow and a chaotic October that will no doubt push my limits and Google calendar capacity. I am full of sadness but gratitude that I was able to take this much time off to nurture myself post-surgery. But of course, this blissful time was more than healing, filled with unexpected adventures including being attacked and bit by a dog and acquiring a brand new port. Who would have thought I would collect so many new scars?
TO THE SHORT VERSION!
When I first started planning breast reconstruction two years ago, I thought: winter. Easy excuse to miss awkward family gatherings (sorry, can’t pass the mashed potatoes, I’m recovering from surgery) and work would be at its slowest. The only con was getting over the snowy pass to Seattle. But by this point in my life, I know plenty of adults with four-wheel drive and a death wish. Where there’s a will, there’s a Subaru.
Then life said, “No, try again.”
First, a hurricane destroyed saline bag stocks, which apparently put boobs on backorder nationwide. My chop date got bumped. Then in January, my calf decided to audition for “Final Destination” with a blood clot, which bought me another six month delay. At that point, I figured the universe was just messing with me for sport.
By June, I’d resigned myself to calling for a November surgery slot. A co-worker asked why November, and I explained my “skip the holidays” master plan. She pressed: “If you could have it this summer, would you?”
Would I? Summer is my season. Why would I trade hikes on Badger Mountain dodging snakes like Indiana Jones for pain meds and endless reruns? But an hour later and a single phone call, fate sealed it: end of July surgery. And honestly, it was the best decision I’ve ever made.
The last two months have been endlessly joyful. Sure, my body is permanently Frankenstein’d, but I finally got my foobs and faced down some of my biggest fears. I learned how to dismantle my need for routine and replace it with choice. Mornings could be slow, with coffee and chocolate collagen while birds looted my sunflowers like tiny winged burglars. Fridays meant watermelons from the farmer’s market, evenings meant painting and talking art with friends, and afternoons were for tuna sandwiches and TV with my mom (a sacred ritual we didn’t know we needed). I also got to know every feral cat in my neighborhood. I’d go on walks, film them like I was documenting a nature show, and hand out nicknames like candy. Somewhere in between all that, I went to a cadaver lab at my sister’s work conference and casually hung out with dead bodies for an afternoon, and then balanced it out by screaming along to T-Pain at the Washington State Fair in Puyallup because he is, without question, a national treasure.
After everything cancer has taken, I finally cultivated something new from what was lost. This might go down as one of the best summers of my adult life.
But even great summers come with lows. My lymphedema is the worst it’s ever been. My body dysmorphia greets me every time I get dressed. I’m still swollen and scarred. Oh, and I got attacked by a dog and had to get a tetanus shot. To be fair, maybe the dog just sensed I was already stitched together like a chew toy.
Of course, the universe wasn’t done with its plot twists. Just as I was getting ready to say my summer goodbyes, I ended up with a surprise surgery.
It started with a blood draw fiasco. My oncologist wanted a circulating DNA test like yesterday, even though I had regular labs scheduled a week and a half later. That single draw spiraled into failed access of my port, an overnight TPA, countless pokes on both my arm and my hand from my favorite nurses to no avail. My veins basically ghosted us. We joked that I was dead, but the truth is, I’m just a terrible poke. And because of my lymphedema, only my left arm is an option, which makes IV access a gamble. My nurses advocated the hell out of me to get a long awaited dye study (I originally asked for this back in January), which revealed that Harry Porter and the Prisoner of Cancerban was indeed blocked by a fibrous sheath. Surprise, surprise. We were at a crossroads: remove it completely, or remove it and place a new one, this time on the right side of my chest.
I made the decision and asked to have one last surgery. Literally the next day, I had a call to schedule surgery for Tuesday. The universe received my manifestation of having this done before going back to work and I can’t help but wonder when my manifestation magic will end. This surgery? Honestly a 10/10 experience. I was consciously sedated, the team was amazing, and yes, I got to try fentanyl. It wasn’t as cool as I thought it might be. We even gave Harry Porter one last hurrah as the IV access point before retiring him for good.
As for the new port? I held a naming competition on Instagram Stories, and despite some excellent suggestions, I couldn’t escape the Harry Potter theme. Meet Lord Voldemort, he who must be flushed. (Thanks Heather for the name lol.)
Summer is now fall and I already miss the warmth and comfort with a season of life that gave me so much hope. Tomorrow I go back to work, and Tuesday I’ll be back in the infusion chair for my last Zometa treatment. My bones are going to hurt like a bitch, but at least it’s the final time. To mark the occasion, I made little brown butter, bone-shaped Rice Krispies treats to hand out to the nurses because if my skeleton is going to ache, we might as well have snacks. We’ll also get to test-drive Lord Voldeport for the first time.
By then, I’ll probably have my circulating DNA test results too. I’m crossing everything I can cross that I’m still NEAD. I’m still on my oral chemo and hormone therapy, still doing the day-in, day-out grind of survivorship, but right now I’m mostly thinking about how grateful I am.
Every single person who showed up for me these past two months via Meal Train, visits, chats, texts, calls, kept me from turning into a full-on couch potato. Friends who came by to clean my house and yard so I could focus on healing. My mom and sister, my roommate, my co-workers, my nurses, my feral cat audience. You all made this endless summer possible.
Cancer is the worst club to be in, but it has the best people. And because of you, I’m here stitched together, still healing, still choosing joy, still alive. Thank you from the bottom of my little cancer heart.

y u no be my friend??? 
80085 
sick dog bite, bro 
~i am an artist lol~ 
Lord Voldeport 
summer’s favorite gemini Today’s song lyrics of the day are brought to you by Lana Del Rey.
“Think I’ll miss you forever
Like the stars miss the sun in the morning sky
Later’s better than never
Even if you’re gone, I’m gonna drive (drive), driveI got that summertime, summertime sadness”
– Summertime Sadness (Lana Del Rey Vs. Cedric Gervais), Lana Del Rey, Cedric Gervais
-
August 21: Phase one complete
Fast facts (if you don’t have time to read the full post): 1,047 days after my double mastectomy, I finally had my DIEP flap breast reconstruction surgery! It has been a long time coming after a mandatory year waiting period, ups and downs with oral medications required to keep me alive, and two failed surgery attempts. My body and mind are grateful I made it to another milestone, like a swimmer out at sea finally finding a buoy to rest on, but there is so much swimming left to do.
TO THE LONG VERSION!
ACT I: Arrival
“Okay, can you please tell us one final time your name, date of birth, and what you are having done today,” the masked human said as she diverted her eyes from me to a new task. This question has almost become a mantra. Every appointment I have had the last three and a half years requires me to answer this multiple times. I’ve turned it into a melody, like a bird song. It is my guide and secret pass code to unlocking my destiny. I looked around for a brief moment, taking in the sterile room. The overhead lighting looked like a brightly lit octopus, tentacled arms ending in bulbs illuminating the room. Three other masked humans awaited me next to a long uncomfortable looking bed. The first masked human came back, wheeling my bed closer to the second. I took a deep breath and could feel the dam behind my eyes ready to burst.
“My name is Madison Evangelista, six, seven, nineteen ninety two.” My breath caught in my throat and everyone in the room turned to look at me. “I am finally here today for my…. DIEP flap surgery.”
Over the past three years I have tried to imagine what that moment of making it to surgery would feel like, but my imagination has always come up short. What I thought would be this defiant moment of choosing myself and a feeling of freedom and reclamation, mixed with joy and a fucking middle finger to the last three and a half years, turned out to be a cloud of fear in a sterile blank space. Cancer only gives you two choices: do or die. And even that is an illusion of choice, especially at stage IV. Coming to terms with my “choice” to “do” and reconstruction being part of that would seem like a win, but it also is just another mountain I have to climb, another sacrifice to give.
As the anesthesiologist administered the happy juice into my IV and my train of thoughts began to disperse, I felt my fear skirt to the sides of my brain. My eyes became heavy and the masked figures stared at me as I drifted far, far away.
“Fuck,” I said quietly.
ACT II: Unreliable narrator
Some of my favorite online videos are the ones of people coming out of anesthesia. Who are we when we are the least inhibited? Luckily, I had an inkling of who I am and she is the most aggressive version of my most inhibited self: concerned about pleasing, giving, and being the best worker.
In high school, I had all four of my wisdom teeth removed and I was put under for the procedure. Although my recollection of the situation was foggy, what I did remember was reinforced by witnesses of me coming out of anesthesia: I profusely thanked the surgical team for “not hurting me” (I am extremely needle phobic and of course encountered several needles in order to have my teeth removed) and I asked to write a thank you note for the team for their care and kindness. The paper was a bunch of well-intended scribbles and they let me take the paper home for future me to enjoy.
This time as I clawed my way out of anesthesia, a large feeling of dread sat on my chest. I was very upset, but I told myself it was all internal dialogue. Nobody needed to know about the shame I was carrying: I did not finish a bookmark job at work. My team would suffer because I failed to finish a task before I left! I was a bad worker.
Out of respect for my shame, I refused to open my eyes. If I can’t see, people cannot see how badly I fucked up. Also my eyes felt so heavy, so crusty. I can talk and have my eyes closed, I thought to myself. I am gifted.
I became a blind baby bird as my best friend fed me ice chips as she chatted away on the phone. Who was she talking to? Why wasn’t she paying attention to me??? And then someone suddenly peeled back my eye ball and my world was a blurred mess. Baby bird was upset now. No no. Keep my eyes closed, I begged. “You need to open your eyes,” someone said. No I don’t???
Suddenly, a warm liquid sat on my lips. Bad chicken broth, I thought. Who would feed me bad broth??? Is this punishment?
“I’m going to throw up,” I proclaimed. My best friend shuffled around looking for a vomit vessel. A round bag appeared just in time.
“I threw up,” I said in my baby voice.
She patted me on the head. I am a baby bird, I thought.
ACT III: The real story

Turns out my internal dialogue about work was external. I was crying my eyes out over the bookmark project at work and I refused to open my eyes at all. The nurses forced my eyes open to make sure I was responsive. But I was just an upset mess, distressed about work and preserving my dignity. My best friend was playing the role of translator and historian, informing everyone that I had made it out alive of the originally 420 minute scheduled surgery that instead ran for 9 hours. I was doing well, despite my need to keep my world dark.
I had finally made it to the DIEP side.
ACT IV: They say that dreams can come true, but forgot to mention that nightmares are dreams, too.
“I am so sorry but we have to move you into a shared room,” the nurse said. “Another patient has an infection and needs this private room. Is that okay?” My world still felt dark and hazy. My best friend was gone. What time was it? I didn’t fully understand the situation, but somehow the most accommodating version of myself still existed, even in a drug-induced haze.
“Of course,” I said. Did I have any say to actually say no? Who would say no? I didn’t fully understand the situation I was in either. I just wanted my eyes to remain closed.
The only other memory I have of the transition is a tunnel-like feeling in my brain. I am guessing that is from being wheeled down the hallway to my new shared room. Someone else was on the other side of the curtain, a fresh patient. Maybe we will be friends, I thought, and went back to sleep.
“Hi, I am here to take your blood work,” a little voice creeped into my brain. Time was melting into itself. How long had I been there? Blood work? Why? Is this one of my nightmares? A young woman sat next to me, putting on her blue gloves. The rubber snapped aggressively against her skin. I suddenly jumped into consciousness and self advocacy, a gut response conditioned by medical trauma. “I am a really really tough poke and hate needles,” I told her. She put the band around my arm and began pulsing it for a vein to appear. We chatted and I learned she was fairly new. Several minutes went by before I told her she could prick my fingers and try that way. I shared the lore of the inability my IV team had before surgery to find a suitable vein. They used the vein finder and ultrasound before successfully inserting a needle. That permission was a mistake. The next fifteen minutes was spent milking my poor fingers of blood. She was the kindest human, but holy shit what a way to wake up and finally be coherent.
Needle karma is a thing for me. Any time I have ever taken the “easy route,” needles come back ten fold. Another phlebotomist appeared an hour or so later.. My finger blood had clotted and they needed more blood. I once again shared my needle phobia and tough poke predicament, but this phlebotomist was back for revenge. She found my one good working vein and was in and out in a matter of minutes. Was this going to happen every day, I wondered? If so, I was in for a rough couple of days alone.
ACT V: Reality
The first time I had surgery was when I was six years old to have my adenoids and tonsils removed. The second was my port placement. I guess technically my wisdom teeth count, but I file those under a special category: not life-saving, just inconvenient.
By the time of my mastectomy (or, let’s call it what it is, my breast amputation) I was no stranger to what I call quick chops: you’re in, you’re high, and you walk away an organ short. Well, not always an organ. Once I walked away with a nifty device in my chest and the inability to poop for days.
My mastectomy itself was uneventful. No funny anesthesia stories were caught on camera thanks to COVID restrictions. Jose dropped me off. My mom and sister picked me up. I do remember wearing my unicorn breast cancer socks and waking up one sock short of a good time.
Before the amputation, the nurse placed an IV in my right hand, my cancer side. The surgeon later told her it needed to be in my left because the cancer was on my right. Since I’m a tough poke, everyone agreed they’d move it once I was under. After surgery, I have this vague memory of someone saying it had to go in my ankle, but without a coherent witness, it is just another myth and legend stored in the back of my brain.
What I was looking forward to most with this surgery was the four day hospital stay. I’ve never stayed in a hospital for more than a half day, if that. Maybe I’ve consumed too much “Grey’s Anatomy,” but I envisioned how much fun I could have befriending all of the nurses and eating weird hospital food. Maybe encounter a hot doctor? The world was my oyster.
Instead, I spent four days learning how to build a pillow fort on a recliner chair, pretending I was a NASCAR driver as I pushed my little walker around the nursing station, making inside jokes with the nurses, protesting hospital food, and wondering why my hospital roommate was having a rough go.
The first night I barely slept. I was being checked every hour, maybe every other? I lost track. Between the saline drip, the catheter, the IV machine beeping at odd hours, and nurses rotating through like a pit crew, I felt like a science experiment. My roommate and I never spoke, but you know when the air feels clipped, like someone is silently annoyed? Especially if her husband was there and my IV machine started screeching. Once, I’m pretty sure she called the nurse on me because I wasn’t awake enough to notice.
Then there were the heparin shots. The first two-ish days, every four hours without fail, a nurse would slip in, take my vitals, check the IV bag, hand over meds, and jab the back of my left arm. Because of lymphedema on my right side, my poor left arm was the only option. By day three, it looked like an overripe peach, covered in purple and yellow bruises blooming in every direction.
Meanwhile, my roommate was declining. I never knew exactly what she had done, but I think she had a chest tube for her surgery and it caused her to cough a lot, her oxygen kept tanking (even though she had no other symptoms and she said she was fine), and she was constantly surrounded by x-rays, blood draws, and urgent whispers. If I was the NASCAR driver doing laps with my walker, she was the pit stop that never ended.
I ended up being released on Thursday and it was a bittersweet goodbye. I honestly had a pretty good time, which I think people might think I am crazy for saying. I was so grateful to be there. The nurses were top-tier emotional support humans, my surgeons did an amazing job (the nurses said this is some of his best work!), I didn’t die or get sick, and I walked away feeling like hospitals are not all bad. But I will say the food is.

guess how many pillows are behind me? 
The worst food I have ever sampled. It was mystery meat with inedible potatoes and bread??? ACT VI: A place I’ve been before
My mother stands before me, milking the drain tubes and emptying the grenades of fluid into little plastic cups. She writes the numbers down in her bubbly half cursive, half print font. These numbers are our key for unlocking the next milestone of healing.
I peel off the binder and the compression bra, the fabric stiff with scabs, and stand naked in front of the mirror. My reflection is swollen and strange, stitched and glued, a body I half-recognize. My mother doesn’t linger on it. She moves to the shower, runs the water, waits for steam.
She calls me in.
I lower myself onto the chair, ribs tight, belly tugged, arms short and stiff as if my muscles remember what they were after the mastectomy. My mother lifts the shower head, tilts it over my back, and the water runs down me in hot rivers.
The relief is instant. My back unwinds, the aches dissolve, and for a moment the water feels like cure, like blessing. She moves slowly, dragging the spray across my shoulders, over my legs, rinsing me as if I am both fragile and sacred. I close my eyes.
It is humbling to be bathed by her hands, the same hands that once bathed me as a child, the same hands that survived their own cancer. The water patters against the plastic chair, against my scars, against the silence.
When she is done, she gingerly pats me down, wraps me in a towel and helps me stand. I catch myself in the mirror again: not healed, not whole, a stranger in my own body.
A place I’ve been before. And yet, not the same place at all.
ACT VII: 24 days later
A week before surgery, I drove up to Olympia to celebrate my old roommate’s one-year salon anniversary. As a friend, I couldn’t have been more proud to be there and also provide my photo services to her and her team. I nibbled on charcuterie, making small talk, when in walked a woman who seemed to carry her own weather system. The tarot reader.
I’ve had my cards pulled before by one of my closest friends. I am always in awe of her interpretation and gifts, but I knew this could be quite different. This woman knew nothing of me: nothing of the tumors or the pills or the broken pieces of my life. Let’s test her gifts, I thought. With my little cheese plate balanced on my lap, I sat across from her and let the cards fall.
I couldn’t tell you every card she flipped, though The Tower burned itself into my memory (of course). What I do remember is her voice, steady and certain: “You’ve been through a lot this year, but everything you’ve overcome has led you here. Without the breaking, you wouldn’t get to this next thing. Right now, anything you manifest is yours. The universe is listening.”
For non-believers, you might think that sounded like some generic fortune-cookie bullshit, but I swear it wasn’t. This wasn’t vague “new beginnings ahead” energy. This was my messy-ass life laid out in cards. The first five months of the year had nearly leveled me. My marriage crumbled. My body buckled under Verzenio. A blood clot delayed surgery and left my leg looking like it belonged to a pissed-off balloon animal. I was sick, broken, and unmoored. But then: my roommate moved in. We flew to Japan. I switched to Lynparza. Slowly, I began to piece myself back together.
And now, 24 days post-surgery, I find myself staring at these scars not just as damage but as doorways. My surgery date wasn’t just a box checked off a calendar; it was a hinge. A plot twist in a story I thought I already knew the ending to. For the first time in three and a half years, I feel something more than survival. I feel roots spreading. I feel branches reaching. I feel like maybe, just maybe, something for once can go right.
Of course, that doesn’t mean it’s been easy. This surgery has been as much of a mind fuck as chemo and radiation, just in a different flavor. Every day is a different story. Some days I glimpse the promise of what’s coming; other days all I see is destruction and disappointment. I’m swollen. None of my clothes fit right. My scars are fresh. I’m bruised and tight. I was foolish to think that loving this new body would be simple. Instead, it feels like another betrayal. I miss the one I left behind. I miss my freckle below my belly button. My radiation tattoos have shifted. I even have pubic hair sprouting on my foobs from the skin transfer. The constellations that guided me for 3 years are gone, and I’m once again adrift.
I lived almost 3 years breastless. Before that, I spent 30 years in the same body. And it took this stupid-as-fuck diagnosis of breast cancer to drag me to the brink of death, strip me down, and then yank me back just so I could learn… what, exactly? That I’ve developed Olympic-level disassociation skills during blood draws? That traveling beats spending money on cars? If you were hoping for some perfectly inspirational takeaway, I’m still searching for that magic.
But I do know this: life is short. It is later than you think. And I am grateful to be alive in a time when science could stitch me a second chance. Science never promised easy, but holy hell, it is incredible. I mean, have you seen my foobs?!
Epilogue
According to my insurance claims, my hospital stay and surgery were billed at $205,232.92. Because I had already hit my out-of-pocket max for the year (shout-out to my multi-visit ER adventures this past spring), I now owe nothing for this wild, expensive chapter. That relief is thanks not only to my excellent insurance but also to the Women’s Health and Cancer Rights Act of 1998 (WHCRA), a federal law requiring group health plans that cover mastectomies to also cover breast reconstruction. This protection includes rebuilding the affected breast, surgery for symmetry on the other breast, prostheses, and treatment for complications like lymphedema.
But not every breast cancer patient easily gets this outcome. Right now, many women are sharing their stories of being denied coverage for reconstruction, forced to battle their insurance for something that should be a given. I’ve been lucky; my insurance has, for the most part, met my breast cancer needs without a fight. But that’s not the reality for far too many. No one should have to shoulder the financial or emotional toll of pleading for life-altering, medically necessary care. Coverage for reconstruction after mastectomy isn’t a luxury. It’s a right, one we need to defend, enforce, and expand so that every patient, regardless of their insurer or income, has access to it without question and with ease.
If this matters to you, learn about the WHCRA, share it widely, and support organizations pushing for stronger enforcement and broader protections. Groups like the American Cancer Society, Breastcancer.org, Living Beyond Breast Cancer, and the National Breast Cancer Coalition are working every day to protect these rights and close the gaps in access. You can also read the WHCRA fact sheet from the Centers for Medicare & Medicaid Services to understand exactly what’s covered. Patients shouldn’t have to fight for the care their bodies and lives depend on.
Today’s song lyrics of the day are brought to you by Black Eyed Peas.
“My love, my love, my love (Love)
You love my lady lumps (Love)
My hump, my hump, my hump (Love)
My humps, they got you” -
July 13: Magic 8 ball says… try again.
Fast facts (if you don’t have time to read the full post): Once again, I am happy to report that my most recent scans show I am NEAD, despite the turbulent first five months of the year. With that peace of mind and a DVT-free calf (for now… and hopefully moving forward!), I gave myself permission to finalize a surgery date for a third attempt of breast reconstructive surgery. I also had my second opinion appointment and I am left with more questions than I am with answers, but I received the clarity I sought. I quit Verzenio (bye bitch) and I am back on Lynparza. Poison is my friend. Oh and I also went to Japan. LOL. Who the fuck am I?
Countdown to reconstructive surgery: 15 days
TO THE LONG VERSION!
Growing up, my bedroom had mirrored closet doors, installed after a suspiciously persuasive campaign to replace the original brown ones. I don’t know how I convinced my parents, but once they were in, those mirrors became sacred real estate. Every friend who visited was invited to sign their name and leave a message in dry-erase marker. The pubescent graffiti would line the edges of the mirrors, leaving plenty of room for iconic Myspace selfies and outfit checks.
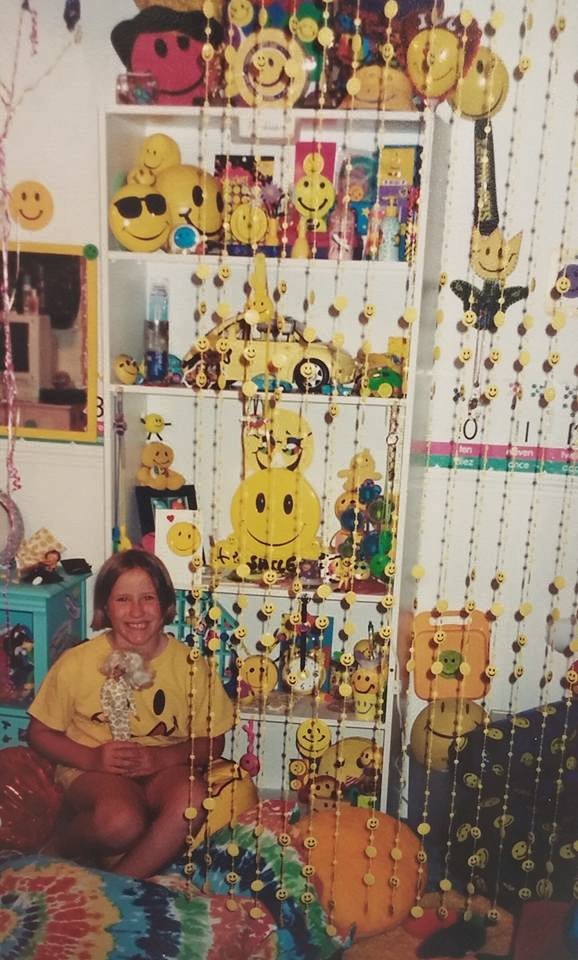
Why you so obsessed with me??? But the same mirrors that acted as my guestbook were also my biggest bullies. I’d stand naked in front of them, tugging at the soft edges of my hips, stretching the “muffin tops” toward my back to picture what I’d look like with a flat stomach. No matter how many laps I swam, how little I ate, or how tightly I trained my body to stay sucked in, my stomach was the enemy. I was obsessed with my belly button, too, convinced it was too big, too oval, too wrong. I’d stretch the skin around it upward, silently bargaining with the skinny gods for a flatter stomach and a cuter navel.
My body dysphoria has worn many faces over the years, evolving through adolescence and adulthood like some shape-shifting shadow. But it shattered the night I shaved my head after my second round of chemotherapy. In that moment, the cruel little voice went silent. For the first time, I saw myself clearly. My body was no longer a project, a performance, or a problem to solve. It wasn’t shaped by trends or peers or some imaginary version of who I was supposed to be. My body was dying, and I was trying to save it. Since then, I’ve never looked at it the same way.
But acceptance isn’t a straight line. Some days I feel grounded in my body, at peace with my scars and flat chest. Other days it’s like I’ve time-traveled back to the first few months post-mastectomy: raw, disoriented, and unsure of who I am in this skin. That ebb and flow is something I’ve learned to live with.
Still, I’ve been moving toward breast reconstruction. For many breast cancer patients, it’s described as a return to normalcy, a reclamation. A quiet (or not-so-quiet) fuck you to cancer. You took my breasts? I’m building new ones. It’s defiant, healing, complicated.
Vanity feels different now. I’m not as focused on how I’ll look in a top or what others will think. What occupies my mind is the healing: the cut that will run from hip to hip. The weeks of recovery and the stop in my routine. The permanence of a body altered again. I worry about what it will feel like to see my new scars and if I’ll recognize myself when I do.
And then there’s the belly button.
I’m losing it.
A body part that’s been with me since birth, proof of a life-giving connection to my mother, the soft center I once poked and pulled at in front of those mirrored closet doors. It’ll be gone. Removed and remade. Technically, I’ll get a new one. Surgically sculpted. But it won’t be mine. And so many patients have complained that their belly buttons look like little fucked up cat butts. There’s something deeply strange and a little sad about saying goodbye to a body part so ordinary, so permanent, so… primal. And one that I thought was ugly for like majority of my life. And now I could end up with a more fucked up one?!
Sometimes I think about my childhood self, tugging at her stomach in the mirror, convinced that changing her shape would change her worth. It’s surreal to now be preparing for a surgery that will literally reshape my stomach in order to build new breasts. I can see myself clearly now: scars, strength, all of it, but I’d be lying if I said I wasn’t scared. Scared of what this decision might do to my mental health. Scared of making a change for the wrong reasons. Scared of letting go of the version of myself who has been visibly, unapologetically a cancer patient.
This surgery feels like the final step in not looking like someone with stage IV breast cancer. When I’m dressed, no one will know. No more sideways glances. No quiet stares at my chest. And while that kind of anonymity might bring comfort, it also brings a quiet kind of grief. For the past three and a half years, this outward identity has exposed me and at times, made me feel deeply alone. But I’m not sure what feels heavier: being visibly marked by cancer, or blending in so completely that no one sees what I’ve been through?
Emotionally al dente. That’s how I’m feeling these days. Just tender enough to know I’ve been through it, but still holding my shape well enough to pass as a functioning human again. This spring wrecked me. I went to the ER more times this year than I ever did during active treatment, took my fragile little body to Japan, and somehow, in the middle of all that chaos, planned and pulled off the third annual Madison & Friends fundraiser, raising over $9,000 for the Tri-Cities Cancer Center.
I also managed to sneak in a second opinion at Fred Hutchinson Cancer Center in Seattle (one of the top cancer treatment centers in the country) and got a pretty unexpected hot take on my current treatment plan.
The provider I saw mostly agreed with the approach my oncologist has me on, except for one critical difference. Back in April, my oncologist took me off Verzenio, aka the drug that gave me unpredictable diarrhea and absolutely tanked my immune system. That drug was supposed to be a two-year stint, but she decided to stop it early, saying it had “failed” because of my .06 Signatera test in November. (In cancer-speak, “failure” usually means recurrence, which I thankfully haven’t had, but still, she pulled the plug.) And if you remember that conversation, she was wishy washy as fuck about that at the time. One month she said it didn’t matter, and then the next she said it did…
So, she put me back on Lynparza, the oral chemo I was on from 2023 to early 2024. It’s gentler, and honestly, I feel like a functional human being on it. No public restroom roulette, no hiding from germs like I’m in a post-apocalyptic bunker. Just…life. And as of my most recent labs, I am tolerating it super well and I don’t mind it at all.
But the Fred Hutch provider had a very different opinion. She recommended stopping Lynparza, not because it isn’t working now, but because if I ever do have a recurrence, I won’t be able to use it again. It’s more effective as a treatment after recurrence, and if I “burn it” now, I lose that option. Instead, she suggested going back on Verzenio for another year or switching to Kisquali—a related drug that has similar outcomes in long-term survival when taken for three years. Oh and she said she thinks Signatera is not a great way to monitor for recurrence. She doesn’t even use it. I was like girl, WHAT.
That was not the conversation I expected to have.
And honestly? It’s a hard sell. Choosing to go back on Verzenio or try Kisquali means willingly wrecking my quality of life, for the sake of long-term odds that may or may not even apply to me. Lynparza is treating me kindly. I can go out, be around people, and feel like myself. But knowing it’s not the preferred drug for someone being treated as stage III (which they are still treating me as such because of how few of mets I had in my spine) makes this whole decision feel…impossible. Do I choose the drug that lets me live my life now, or the one that might help me live longer?
We also talked about family planning. The second opinion provider was incredibly supportive of me keeping my ovaries and, if I choose to, having children someday—after at least five years on hormone blockers and completing a stint with Verzenio or Kisquali.
That conversation cracked something open in me. It felt human. Hopeful. Like someone finally acknowledged that I’m still a whole person with ambitions and dreams and a desire to live this second life, not just a body to be treated. But now, two months later, I still don’t know where to place that hope. I carry it around like a fragile secret: beautiful and terrifying. Because how do you plan for a future you weren’t even sure you’d get to imagine?
And truthfully, I haven’t brought any of it up with my current oncologist. Our communication has not felt very open lately, and at this point, I’ve developed some real trauma responses when it comes to interacting with her. I’ve been cornered in appointments, pressured to remove my ovaries, dismissed when I brought up concerns like my DVT and long-term management of cancer side effects. And each time that happens, something in me retreats a little further. It’s not just frustration. It’s grief. It’s the emotional fallout of being dismissed by someone who holds your life in their hands. When your doctor treats your body like a battleground but ignores the person inside it, it chips away at your ability to feel safe in your own care.
Once again, I’m left with more questions than answers and at this point, I’m living life strictly one day (and one belly button photo) at a time. I’m soaking up every CrossFit class I can, savoring my independence while I’ve got it, and paying tribute to my soon-to-be-retired navel like it’s a hometown hero.
If you’d like to support me through this next wild chapter, a very kind friend has set up a Meal Train to help me out while I recover. I won’t be able to do much for myself the first few weeks (think T-Rex arms and naps galore) and I’ll be out of work for about eight weeks total.
To the friends, family, internet strangers, and relentless little weirdos who keep showing up for me: thank you. I’m only still here because you refuse to let me peace out.
Here’s to healing, hot girl summer (from the couch), and finally becoming the boobalicious girl of my dreamz.
Today’s song lyrics of the day are brought to you by Incubus.
“Sometimes, I feel the fear of
Uncertainty stinging clear
And I, I can’t help but ask myself
How much I’ll let the fear take the wheel and steerIt’s driven me before, and it seems to have a vague
Haunting mass appeal
But lately, I’m beginning to find that I
Should be the one behind the wheel” -
April 10: Negotiations
Fast facts (if you don’t have time to read the full post): This week is Adolescent and Young Adult (AYA) Cancer Awareness Week and I feel compelled to write you a blog post. Surprise, surprise?? Most of it will be just about my thoughts and feelings about this week, but some of it will be about my most recent cancer appointments. I hope you stay for it all. Thanks for reading.
Countdown to Tokyo, Japan: 22 days
TO THE LONG VERSION!
5:54 pm: I open my Instagram app and the feed refreshes. There’s a selfie of a cancer thriver I’ve followed for a while now. I scroll to read the caption, only to find that it is a letter to her followers.
“Final update: If you are reading this, then I have left earth side.”
She thrived for three and a half years. She was 33 years old.
Mermaidwithcancer was one of the accounts I started following through a campaign last summer I was invited to be part of that focused on stage IV breast cancer thrivers. I did it because I was looking for community and sure enough, I found them (and they found me!) So many are advocates in their home towns and virtual spaces, raising funds and awareness for a disease that can be so damn relentless and unforgiving. These women never aspire or want to be inspirations; they all just are trying to make lemonade out of lemons. And most of the time that lemonade is tart as hell.
Still, no amount of sugar can soften the truth: we are so often expected to battle, to be brave, to bear it all in combat terms. In the cancer world (in general), the metaphor of “fighting” is often used.
War.
Winning.
Ongoing.
Battles.
Loss.
Lose.
Today, a friend I met online sent me a message about a video I shared to my story for AYA Cancer Awareness Week and she shared the story of her daughter’s best friend who “negotiated” with cancer in her 20s.
Pause.
Negotiated. With. Cancer.
I rolled that around in my head. Cue lightbulb moment.
6:03 pm: I’m staring at my phone in the bathroom, trying to figure out where all the fucking ants on my bathroom floor are coming from, and having this weird argument in my head that she didn’t lose her battle (because I *hate* the metaphor of fighting), but the terms of the negotiation somehow had ended and I am half crying, half laughing at the change of language and wondering if mermaidwithcancer would agree with the reframe. (This sentence was meant to be a run-on thought. My grandma is rolling in her grave over my disrespect of proper English writing and the lack thereof.)
6:37 pm: Negotiating. Negotiations. Negotiate.
6:44 pm: My body is rude as hell. I don’t fight. I negotiate.
I broker peace with injections that shut down my ovaries.
I sign contracts in side effects.
I take hard drugs for the chance of soft hope.
I infuse myself with poison and call it progress.
I live with pain like it’s rent I owe.
I surrender the idea of “healthy” in exchange for “here.”
I swap scans and blood draws for a sense of security.I am just a woman at the table, trading pieces of herself for a shot at more time. And I bring my whole self to it. Every damn day.
This does not make me brave. This makes none of us brave.
We bargain. We bend. We give up parts of ourselves we didn’t know we could live without. We make impossible trades for a few more tomorrows.
Wouldn’t you?
7:08 pm: I turn 33 in two months. In August of this year, I will hit my three and a half year milestone of living with this fucking backwards disease, and this week just makes me feel like a bleeding heart.
AYA Cancer Awareness Week puts a spotlight on stories like mine. Like mermaidwithcancer. Like ours. But sometimes that light feels too bright. It exposes everything I try to tuck away just to get through the day. And then I remember awareness isn’t about spotlighting strength; it’s about telling the truth.
It’s about honoring the ones who ran out of things to trade.
It’s about making space for the ones still negotiating.
It’s about reminding the world that young adults get cancer too and we are not just numbers or hashtags or statistics to be inspired by. We are underserved, unresearched, and under resourced.We are human.
We are exhausted.
We are still here.And sometimes, being here is the most radical thing we can do. And when we’re no longer here, it doesn’t make us less. It means we gave everything we had.*
*In memory of mermaidwithcancer and the many other stage IV breast cancer thrivers we have lost. Rest in power. #StageIVNeedsMore
The month’s go by too quickly. Yet again, just a couple days ago I found myself back at the cancer center for another round of blood draws, a visit with my oncologist, and ended with a (surprise) infusion and monthly injection. Since this blog post has already been a doozy, I will try to make it less intense and more… I don’t even know??? Cancer is always intense and this narrative I am currently in just keeps getting WILDER.
I embodied the Brave Little Toaster on Monday. Harry Porter (my port) FUCKING DID NOT WORK AGAIN. I do not understand what the point is to have this little noodle strapped into my aorta if its not going to give the people what they want. And just in case you don’t know, we want blood. Lots of it. Some for labs and some for sacrifice to the trash gods.
Normally I force the nurses to work on me for like 30 minutes and then TPA me, but this time around we all were just defeated and I accepted my fate of having my blood drawn from my left arm. I have not had my blood drawn that way since one of my chemo sessions in 2022. This was a big fucking deal. One of my favorite nurses held me to her chest as I bawled my eyes out in defeat, another sprayed freezey spray on my arm, and another poked me.
For the record, this did not feel like a negotiation where I got anything in return, at least physically. All I got was a bruised ego and even more bruised arm. I didn’t even get a sticker.
But let me tell you… I love my cancer center nurses more than I can ever communicate. These women have been with me since day one and I can’t imagine a better team to help me survive.
After ruining my top tier mascara, I dragged myself over to the next waiting room. Thirty minutes later, I was waiting anxiously for my oncologist. Anxious is probably an understatement. I was ready to throw it DOWN with her if she mentioned the removal of my ovaries again.
Y’all… the conversation with her could have not been more different than last month’s. In summary, no mention of the removal of my baby keepers, I was granted a small break from oral chemo and will officially begin May 12 when I return from my trip, I am back to just a year-long commitment to oral chemo (which aligns with the timeline I was on with Verzenio), and she was happy that I was NEAD.
How is it that the goal post just keeps moving? I like that it is closer, but now I am questioning why it is so close.
Now, what I didn’t know until I had labs was that I had my bi-annual Zometa infusion. If I had known, I would have brought all of my party chemo pod supplies: IV lights, cat banners, and little gifts. Despite the lack of supplies, I was in a klepto mood and stole some tuna and crackers from the snack bar and had another favorite nurse scoop me up some Tillamook cheese for chemocuterie. I just wish I could have had a pod friend to enjoy it all with.
I went back to work for a couple of hours and then made the second trek of the day to Richland for my follow up with my new PCP aka my new favorite medical hero. Now this appointment went way better than expected: we addressed my weird smelling pee (turns out I have a UTI), addressed the pain that I thought was a PE but wasn’t but still lingered (turned out to be a rib out of place), and then I took an A1C test to see if I was prediabetic. I am technically not, but was .3% away from being out of range so…. what gives, body? I also requested a massage therapy referral and received that the next day. Top tier service.
I left feeling like we had solved some problems. Speaking of solving problems… I am waiting for a call back from Fred Hutch Cancer Center in Seattle for a second opinion appointment. If you’re not familiar with Fred Hutch, they are one of the top ten cancer centers in the world! And its just a quick little 4 hour drive. Yay.
To say that my emotions are on a rollercoaster this week might be an understatement. Good news. Sad news. Everything in between.
In the grand negotiation of staying alive, I guess this week I traded blood, tears, and mascara for NEAD, cheese, and a massage referral.
Honestly? Not the worst deal I’ve negotiated.
Today’s song lyrics of the day are brought to you by Linkin Park.
“I wanna heal, I wanna feel what I thought was never real
I wanna let go of the pain I’ve felt so long
(Erase all the pain ’til it’s gone)
I wanna heal, I wanna feel like I’m close to something real
I wanna find something I’ve wanted all along
Somewhere I belong” -
March 25, 2025: It was the best of times, and it was the worst of times.
Fast facts (if you don’t have time to read the full post): Fuck. You guys, I think this is a day where you should skip the fast facts and actually read the fucking post because I feel like the fast facts need context. But if you’re only in the mood for a teaser, here is what the last four months have been like: Green light for surgery, red light for surgery, DVT diagnosis, physical and emotional pain, calf swelling, lots of leg ultrasounds (four to be exact), bullshit from my oncologist about my ovaries and an oral chemo life sentence, and as of four days ago, the blood clots are… gone???
What the actual fuck?! And also to be clear, this post is not to garner pity. I just want to provide some context, clarity, and explanation for why you, dear reader, might have been personally victimized by me ghosting you. (I feel really bad about that, by the way.)
Countdown to last day of Verzenio: 13 days????
Countdown to Tokyo, Japan: 38 days
TO THE LONG VERSION!
In the front of my house, tucked into a corner, drapes a Japanese maple tree. In late spring, summer, and early fall, you can watch it transform from bright crisp green leaves into hues of orange and yellow. The colors are almost like a fall sunset, blazing and gasping on the last breaths of summer.
But in early spring, before the tree even wakes up, you will find long green leaves extending into the rocks next to what I suspect is an old sprinkler box right under the tree. In a matter of a week or two, a little shoot will appear and not long after that, a single tulip will bloom. I love tulips. I love how sweetly romantic they are and how they are always a true indication of spring being on its way. But what I love even more is that I have no idea where this resilient perennial came from. I’ve thought so many times about digging it up and transplanting it somewhere that provides more sun and water, but for what? Every year despite the conditions that it lives in, I get to enjoy my tulip. Why should I ruin that?
This spring, I feel like a tulip. I don’t know how got I placed into the life that I did, why I am next to a shitty old box (cancer), or why I couldn’t be somewhere for everyone to see. Yet, I bloom. I endure. And I ask myself, “What would you be willing to do to survive?” The answer keeps surprising me. Just when I thought I’ve hit my threshold of what I can handle, I reach a new limit, but not without consequence or sacrifice. Every choice of self-preservation requires me to drop something else: prioritizing friendships, keeping the house clean, responding to texts, showing up as close to 100% as I can. I had to let go of a lot this winter to really pour into myself and my health because it was required of me to make it out of this season of life alive.

Three years with breast cancer. I endure. I persist. I’ve learned to carry beauty and grief in the same hands. But more and more, I am learning to live: a practice, a choice, a quiet rebellion, like flowers daring to bloom in the cracks. #cancerversary Here is a little general timeline of what has been going on lately (in a nutshell because it would take up your whole night time routine to cover):
January 13: I was cleared for breast reconstructive surgery despite .06 positive Signatera ctDNA test in November. However, I did have a CT scan at the end of December and it also came back clean. My oncologist basically said that we have to see trends in my blood work in order to determine that treatment has failed and to not worry because everything else was looking great. I walked away relieved and ready to get foobs (aka fake boobs aka reconstruction).
January 15/16: I landed in the ER for extreme calf pain and swelling, only to be diagnosed with a deep vein thrombosis (DVT) and a superficial blood clot on my left calf. Surgery was cancelled, with instructions to call in six months once the DVT cleared. My world fell apart.
January 20: Booked a trip to Japan for the first week of May of this year because fuck being sick. I’ve got life to live.
~Intermission~ Went a whole fucking month as if nothing was wrong. It was absolutely wild. And honestly nice. I really thought things were on the up and up!
Beginning of February: Jose and I separated. Big ooof. I am leaving this descriptionless because I am not quite ready to talk about it.
February 21: Celebrated (Honored? What is the right word here??) my three-year cancerversary. Not dead yet… yay?
February 27: Ended up in the ER once again for swelling and pain in my left leg. Despite being on blood thinners, my DVT was unchanged. Was told not to return unless my chest hurt and/or I had shortness of breath as this could be a sign of a pulmonary embolism, very unlikely on blood thinners but definitely a possibility. How reassuring.
March 8: I made a bold visit to urgent care because I acquired some sort of upper respiratory infection while in the ER. Literally worst cough of my life. Tested negative for COVID at home. Received an x-ray of my lungs while I was there, but no resolution was met despite how sick I had been for over a week at that point. Urgent care defaulted to my oncologist for follow up care. Oncologist defaulted to urgent care. Both decisions resulted in nothing and raw dogging an infection. Cool cool cool.
March 10: One of the worst appointments I have had in the last three years, maybe the worst? My oncologist told me that I was being so anxious about all of my health stuff based on the fact that I had been to the ER several times and have been sick. She feels like being stage IV is making me anxious. (No shit? But also, I am having real health issues??? I normally operate as if I don’t have something inside of me trying to kill me.) And then went on to tell me that she wants me to remove my ovaries this year because I am so high risk (this whole time our agreement was ovaries out by the time I am 40 or if something happens and FYI NOTHING HAS HAPPENED) and she sentenced me to a lifetime of oral chemo (which the plan was after next spring I could stop or at least have a fucking break.) Oh, and she wants to switch my oral chemo back to what I was on initially because this one “isn’t working.” Ironic because in January she said the fucking opposite? She was like well you’re on Verzenio and it is working so go off, get foobs, be free little cancer patient! (Not a direct quote!) I left the appointment in tears and now very determined to get a second opinion. To top it all off, fucking Harry Porter and the Prisoner of Cancerban refused to give blood. I was sent home with blood clotting medicine overnight in my port and instruction to return the next day. Sleeping with your port accessed is super uncomfortable, for the record.
March 11: Returned to the cancer center to have my labs drawn once more. Results showed my initial two tumor markers remained stable and I was (surprise, surprise!) neutropenic. Labs were also collected for my big tumor marker test to compare to my November results. Cue panic.
~Continues to raw dog upper respiratory infection, but was starting to somewhat improve~
March 18: I established care with a PCP! This is a huge positive milestone to hopefully alleviate me having to go through my oncologist for certain things. In a recap, my provider asked me if I was okay based on the appointment notes with my oncologist. I cried because it was so nice to be seen and cared for emotionally about my physical health. I generally do not receive that level of care during my oncology appointments. I am there to be kept alive, not to be kept alive well. For the first time in three years, I felt like an actual patient, not just a body needing saving.
March 19: New swelling and pain began once more in my left calf; an ultrasound was ordered courtesy of my PCP. This also was accompanied with mystery lower chest pain.
March 20: ctDNA results came back: I am still no evidence of active disease (NEAD) despite the .06 positive test in November. However, my chart with my oncologist reflects that my treatment failed, but I am not 100% sure that it actually did. But I am not a doctor, so what do I know?
March 21: I had my ultrasound of my leg at 4 pm on a Friday. An hour later I had results saying the blood clots had cleared but chest pain remained. I ended up going to the ER for a suspected pulmonary embolism (PE). CT scan came back negative for a PE. Left the ER with chest pain (my pain was about a 7!) and no answers other than acute kidney injury on my chart and potential lung inflammation.
March 25: I met with my gyno to have my annual wellness exam. I have not had one since 2022, the day I had an emergency wellness visit due to a large mass in my breast. February 11, 2022 will live rent free in my head forever. It was an emotional visit once more, with my provider kindly emphasizing she wants to help me as much as she can in navigating towards finding a new comfortable normal in my new body. I once again felt emotional and seen by a provider. Jesus. I need a fucking second opinion.
Present day: Although tests show that I am NEAD and I no longer have blood clots, I am still having abdominal discomfort and random nausea. I pride myself on rarely having nausea, so this for me is slightly concerning and I will continue to monitor my symptoms and advocate for myself.
Future plans: On Monday, April 7, I meet with my oncologist in the morning for labs and to be reminded of my indentured servitude to oral chemo and then see my PCP in the afternoon. Double whammy! I will begin Lynparza, a PARP inhibitor, for the second time and tentatively forever. We all know how that went the first time (REMEMBER THE SHINGLES ON MY VAGINA?!) However, I will say that I am absolutely looking forward to not having random life-changing diarrhea. That is my fucking silver lining in my life now: a lack of fucking diarrhea.
Fuck me.
Also, this ~should~ be my final year of Zometa infusions. I have two left in the books. But with my oncologist, you just never know!
Phew. That was a lot.
John Mayer once wrote, “Your body is a wonderland” and I certainly feel like it was written about me, except less sexy, more perplexing, and way less fun. I can laugh and swear and write about the last four months as if it was nothing, but this year truly broke me.
In the darkest points of the night, I greet my grief with open arms. I thought three years in, I would feel farther and farther away from the bomb that blew up my life, but these four months have truly reminded me how fragile my health can be and I can’t help but wonder if I will still make it out alive.
I really fucking hope so.
Today’s song lyrics of the day are brought to you by Lady Gaga.
“You’re so tortured when you sleep
Plagued with all your memories
You reach out and no one’s there
Like a god without a prayer (yeah)” -
December 1: .06
Fast facts (if you don’t have time to read the full post): Ooops it has been 5 months since my last update. Let’s see… in terms of fast facts I have been on Verzenio officially for six months, with a year and a half to go; I went to Europe in September and enjoyed my ~dream trip~; I completed in my first CrossFit competition and also had COVID for the fourth time literally days before; and I was supposed to have reconstructive surgery on November 11 and received a call a couple weeks before surgery that it would be cancelled indefinitely due to saline IV shortage, only for it to be rescheduled for February 3, 2025. It has been a wild couple of months.
Countdown to last day of Verzenio: 546 days
Countdown to reconstructive surgery: 64 days
TO THE LONG VERSION!
Ask any cancer survivor and they can likely tell you the date of their last day of treatment just as easily as they can tell you their birthday. Hell, most can tell you the exact day and time they received their diagnosis. It is hard to forget a life-changing moment like that, with these benchmark dates just as memorable as the quantity of years that pass.
The first five years after a metastatic cancer diagnosis are considered the most crucial because most recurrences of cancer happen within this time frame, and the five-year survival rate is often used as a benchmark to assess a patient’s prognosis; meaning if a patient survives past five years, their chances of long-term survival are generally considered higher.
Each day I feel like I am banking more time in my survivorship fund, but I wonder when life will come back and ask me to cash out. Even as I approach my three year cancerversary in February, the paranoia of cancer ravaging my body once more looms like a dark far off storm cloud, and for good reason.
Every three months I take a blood test called Signatera that compares my blood sample to my tumor sample, looking for the unique “footprint” (for a lack of a better term) that is indicative of my specific cancer DNA. I started taking the test in 2023 shortly after I finished active treatment. My insurance has been a bitch and has been refusing to cover it (each test is about $5,000 out of pocket) but my oncologist told me to take it anyway and to ignore my insurance. Yeeeaaaaaaahhhhh ok. It is fairly new to the breast cancer world, only being FDA approved in the last couple of years if I remember correctly. It feels very science fiction but it is one of the reference tools we have in our arsenal to monitor for recurrence. It is not the end all be all decision maker, but it is insightful and helpful.
Since I started taking the test, all of my tests have come back negative. The little chart reads 0.0 and I get to go back to pretending that I am invincible because I take all the drugs and do all the things to keep cancer away.
That is, until my most recent results.
I went in for labs November 18. We had my normal labs to pull, as well as the three vials that came in the Signatera box. My favorite nurse Jessie saw that my oncologist did not ask to pull labs for my other two (less impressive) labs that also monitor specific proteins in my blood that can be indicative of cancer, but she pulled additional blood for it anyways per my request. I didn’t see a provider and I went and got my monthly Capri Sun stomach stabbing. It was a regular visit with nothing impressive to note other than I did not get my free cheese (and I am still upset about this.)
I haven’t been receiving the results of my Signatera labs the last couple of times I’ve had them done. I don’t know why. For a couple of tests, I received something in the mail about them being negative, but lately I stopped getting any communication and my oncologist would just report back that they were negative. This time around I felt like it would be no different. But on Wednesday, November 25 I received a text at 8:30 in the morning that I could log in to view my Signatera results. Weird, but cool since I am nosy and enjoy that flexibility. I created an account and logged in to see an uptick in my chart and the worlds “Final results summary: Signatera positive” with a flat line of results and a big line up to the .06 range.

Well this is dumb. When I tell you that I spiraled, I SPIRALED. I felt sounds turn to white noise, my hands became clammy, and the air was sucked out of my lungs. Why do terrible things happen to me right before the holidays??! Or on Fridays. The universe really loves to see me squirm. I generally have bad luck with bad news on days that I can’t do much about it. Decidedly, I needed to talk to an adult who was smarter than me. I screenshotted the results and sent them to my nurse friends and then to my oncologist via MyChart. And then I just went emotionally numb.
This was a day I didn’t want to ever have. The paranoia has been justified. Is this is punishment for thinking everything might be okay, that I could be one of the lucky ones? I irrationally rationalized and justified the blip in my blood work timeline as a fault of my own doing, despite the lack of evidence. Even almost three years into this, I feel immense guilt for a disease I cannot control.
Most of the time spiraling gets you nowhere except farther into a land that is hard to come back from, but it worked out on Wednesday. Nurse Jessie (my favorite!) messaged another nurse working with my oncologist directly that day, which triggered a call directly from my oncologist (lucky me) about how I don’t need to worry and that (and I quote) “this is why you are taking pill after pill because you are high risk.” And that these pills will go after anything that is trying to stir up trouble and in three months we will re-evaluate with another test and see what’s up. She said it as if it was of comfort to know that in THREE MONTHS I CAN GET MORE ANSWERS and as if lines of treatment can’t/won’t fail.
I feel defeated. I trust my oncologist. She is aggressive in her approach and has not led me astray as of yet. But something no longer feels right. I am trapped in my body with no way of knowing if, when, and where cancer is hanging out. I have no boobs to feel for local recurrence. If I could reach in and feel up my liver (or any organ, really), I would. All I have is gut instinct and some blood tests and that is it. That little .06 has torn apart any sense of security I had built from surviving up until this point and it has left me vulnerable. I am at the mercy of my targeted therapies and the possibility of false positives. But I can’t help but wonder if it is enough?
I see my oncologist on December 16 and maybe I can advocate for some scans or something. At the very least guess I’ll get more assurance and clarity about what this .06 really means because my oncologist is on chill mode and I am over here planning my funeral. But what’s fucking new?
Today’s song lyrics of the day are brought to you by Linkin Park.
“I let you cut me open, just to watch me bleed
Gave up who I am for who you wanted me to be
Don’t know why I’m hoping for what I won’t receive
Falling for the promise of the emptiness machine” -
More Than a Slogan: Rethinking Breast Cancer Awareness Month
Prologue –
October is a hard month for me and for some reason I have really struggled this year more than the previous two.
I am one of the estimated 200,000 women living in the US with stage IV breast cancer. Is this disease treatable? Yes, but sometimes the disease outruns currently available treatment options. Stage IV is the only stage you can die from. We still have no cure.
The longer I live with this disease, the greater the distance grows between me and the pink ribbon. It is hard to relate to “save the tatas” when you’ve had yours amputated in order to get a chance at surviving. This year I am calling on you all to rethink Breast Cancer Awareness Month. Put stories not slogans at the center of awareness. Start the critical dialogue with loved ones about the risk of breast cancer in your family. Remember to do your monthly self exams and schedule your annual breast exams and mammograms. Learn the signs and symptoms of breast cancer. And most importantly, if you choose to buy and wear pink this month, please do your research and find organizations that donate those profits back to patients and research for a cure.
The following piece was originally published in Tumbleweird’s October 2024 edition.
“Save the tatas!” we all screamed in unison. It was Pink Night at a high school football game. We were decked out head to toe in pink shirts, Mardi Gras-style pink beads, tutus covered in glitter, and our faces were decorated with small pink ribbon tattoos. Was this an awareness campaign night? Was it a fundraiser? I don’t remember, but it always happened in October, and I always went because it was fun to get dressed up monochromatically and ‘support a good cause’. It was a mainstay in the high school program routine. Breast cancer sounded shitty but it also was this far away thing that I didn’t understand at 16 years old. Everyone loves a good theme, even when they don’t know what it really means.
Fast forward to fourteen years later — when my breasts were amputated off my body at the age of 29 with a diagnosis of stage IV breast cancer. I endured 20 rounds of chemotherapy, 28 rounds of radiation, and have been on hard maintenance drugs ever since (and will be indefinitely) that target potential abnormal cells looking to gather and take over once more. For now, my cancer is getting the memo that my body is a no cancer zone, but it often feels like I am on borrowed time and at the mercy of medical advances and existing treatments. We couldn’t save my tatas; and two years into being breastless, it’s hard not to wonder if saving myself was enough.
We’ve all seen the breast cancer awareness shirts with slogans like: “I am here for the boobs,” “Squeeze a boob, save a life,” and “Save second base.” Nowhere in the vernacular of commercialized breast cancer awareness is the life and soul of the breast cancer patient put front and center. The disease has been hijacked by the hypersexualization of breasts, reducing a life-threatening illness to a series of flirty catchphrases and trivializing the very real suffering it causes. This focus on breasts as objects of desire — rather than integral parts of a person’s body and identity — perpetuates a culture that overlooks the physical and emotional trauma faced by those battling breast cancer. It diminishes the gravity of the diagnosis, turning a fight for survival into a cheeky play on words.
This hypersexualization also alienates many patients who feel that their experiences are not being taken seriously. It glosses over the complex and painful realities of treatment, such as the loss of breasts or changes to breasts following a lumpectomy, the fear of recurrence, and the impact on one’s sense of self. For those who lose their breasts as part of their treatment plan, these slogans can feel like a cruel reminder of what’s been taken from them, reducing their struggle to a punchline and insinuating that they did not do enough mammograms or self checks to prevent breast cancer. This narrow portrayal also neglects the stories of male breast cancer patients, further entrenching the idea that breast cancer is only about female sexuality rather than a serious health issue that can affect anyone.
In the process, the true message of breast cancer awareness — early detection, support, research, and survivorship — gets lost. The focus shifts from saving lives to preserving an idealized image of femininity, leaving those who don’t fit this narrative feeling isolated and unseen. We need a shift in how we talk about breast cancer — one that centers on the humanity of those affected rather than on the commodification of their bodies. Awareness should be about more than just saving breasts; it should be about education, advocacy, compassion, and a commitment to supporting those who face this devastating disease.
October is Breast Cancer Awareness Month. As we navigate through this month, it’s crucial to redefine breast cancer awareness beyond the slogans and superficial campaigns. We must challenge the narratives that reduce a life-altering illness to a series of catchy phrases, and instead focus on the real, human experiences behind the disease. Let’s prioritize the stories of survival and those we have lost along the way, the importance of early detection, and the need for ongoing research that could save lives.
I urge you to look beyond the pink ribbons and truly engage with the realities of breast cancer — by supporting patients, advocating for comprehensive care in all stages of breast cancer and survivorship, and pushing for a more authentic representation of this disease. Together, we can create a culture of awareness that honors the lives and struggles of those affected, and work towards a future where no one has to lose their life or sense of self to breast cancer.
-
July 1: Shit happens
Fast facts (if you don’t have time to read the full post): I’ve been on my new nemesis of a drug Verzenio for one month and it has been a shitty time, both literally and figurately. Cancer is truly the gift that keeps on giving. My blood work showed today that I am not making up feeling like crap. My white blood count, platelets, and absolute neutrophils have dropped. All it took was 30 short days to return my body back into a fatigued, sad landscape. Womp womp.
Countdown to last day of Verzenio: 699 days
Countdown to reconstructive surgery: 133 days
TO THE LONG VERSION!
To my sister who most likely will read this… I am so sorry but I promise to treat this story with dignity. This story has haunted me on my Verzenio journey.
My memory has always been poor, now further amplified from chemotherapy and all the drugs I take. Memory recall takes great effort and focus, especially my short term memory. However, there is this core memory I have as a young sprout, sitting in my mom’s maroon mini van with my sister. It is pitch black out and my mom left us in the van as she ran inside a store to get something. Cassidy’s stomach was upset which was a regular occurrence but that night… oh that fateful night something was truly amiss.
If you have decent instincts, you might understand the feeling of knowing that something is about to happen. You don’t know what or how, but you know something is looming. I think I had that feeling that night. I don’t remember much that happened leading up to the climax of this story, but country music was playing softly in the background and we were wearing velvet pants, a perfect scene of two millennial girls in the early 2000’s. Suddenly, a weird scent filled the van and my sister started to cry. I was sitting behind her in the three row van and I peered over the seat to get a look. To my absolute horror, she had pooped in the car, but it was not just any poop. It was severe diarrhea and it was EVERYWHERE.
As the older sister, I panicked and debated whether or not to go into the store to shout for my mother to come back to the van to help. I ultimately stayed in the stink. The next entry of the memory involved arriving home in a state of chaos. My sister was lifted out of the booster seat from her yellow-orange puddle. She was whisked off to the bathroom and I just stared at the mess. I was horrified. How did this happen?
Fast forward to June 26, 2024 and I learned how that night might have unfolded for my sister and I now fully understand the agonizing feelings that those struggling with IBS or other bowel-related issues face on the daily. After starting my new oral targeted therapy on May 31 (read more about it here), I have learned some incredible life lessons: You cannot trust a fart, always know where a bathroom is, and never leave my poop bag at home (the fond name I have given to a repurposed makeup bag that carries Imodium and kaopectate to help when the urge of shitting myself strikes.)
At this point I bet you thought you were going to read a story about me shitting my pants and I am really happy to report that although I have been too close to such fate, I have yet to ruin my leased vehicle (or anyone else’s for that matter.) But the danger of a cramping stomach on the road, the inability to find a bathroom safe enough to hunker down in, is a new fear I live with daily. Yes, you may mock me and laugh (or close out of this tab and cringe in disgust) but diarrhea haunts me in the same ways that tortured ghosts do in haunted homes: always lurking and always a surprise.
I made a grave mistake joining countless Verzenio support groups and forums before starting the medication. I tormented myself with so many stories of patients shitting themselves, losing all of their hair, and their inability to function due to extreme fatigue. The trauma I have from chemotherapy began to claw its way out of the depths of hell that I had buried it in. I had promised myself that I would not allow myself to endure two years of extreme side effects. I don’t think I have the mental fortitude to do it right now. Everything I read just wreaked of violence on my body and I was having extreme anxiety over it.
I started Verzenio May 31, a week before my 32nd birthday, days before a big Pride event in Pasco that I was photographing, and just two weeks away from graduating from my leadership program. No better time to fuck up my intestines and colon than when I am busiest! Everything went well the first couple of days. But by June 3, the day I had my monthly labs and check in with my oncologist, things began their slideway decline. After my morning appointments, I went to a luncheon for work and ate a slice of greasy ass Domino’s pizza. I mean first mistake was eating that pizza when I have been eating so clean, thanks to my nutrition coach. Second mistake was thinking that I was going to be fine. No more than 15 minutes after gobbling down the pizza slice did I find myself releasing a higlighter yellow liquid into the wild. Okay, so pizza was going on my no go list. No biggie. I got this.
But as the month has dragged on, the frequency of what I politely call GI attacks began to evolve. It went from triggered from certain foods, to a pattern of every couple of days I could expect a flare up. But now I have learned that my flares just happen and I cannot figure out what is triggering them or why. I was content knowing I could avoid certain foods and drinks. I even went a strong 5 days without an attack! And then something changed and now I am at the mercy of the universe. I bargain with my body daily to let me be free of the sudden diarrhea and cramping for a social event or outing in favor of a time that I am at home and less vulnerable but do you think my body cares or listens? No. I mean it isn’t really my body’s fault. It is Verzenio holding my cells captive, ruining my immune system and deleting the power I once had over a strong colon. Clenching used to be my super power. I am now a pooping machine and nothing can stop me.
So yeah, June was really shitty and it shows no signs of stopping. Verzenio has diarrhea as the #1 listed side effect, followed by nausea, stomach pain, fatigue, anemia, and leukopenia. There are more, but those are the ones I am currently dealing with. I have noticed I bruise easier and for longer as well, but thank fucking god I have not experienced hair loss. I’ve suddenly gained weight quicker than normal, even without shifting my diet. I dream about napping all of the time again. My immune system is returning to its nonexistent status. Oh, and my hot flashes are way worse now.
But other than that I am… fine. I am alive.
In the grand scheme of things, these are small prices to pay for remaining NEAD (no evidence of active disease.) The goal of this drug is to kill off cancer cells that might be too inconspicuous to detect on a scan, but have the ability to be extremely dangerous if left to their own devices. The longer I go as NEAD, the better outcome, statistically speaking, I have long term. I hate the things I have to do sometimes, but I will always choose the path that give me the best outcome. Life is too great to not.
I have the option to lower my dose, but I do know my oncologist wants me to ride this high dose as long as possible to see if my body can acclimate. I have agreed to go another month raw dogging the toilet bowel in the name of experimentation, but if things continue to escalate (and if I poop myself in any vehicle) I will be asking to lower my dosage. It is preferred for me to stay on this high dose because I am high risk for recurrence so I am trying to negotiate that with my emotional side. You want cancer again or five trips to the bathroom within an hour? I will gladly wear the porcelain throne crown for now.
As I settle into my new temporary normal, I have noticed I am returning back to some of my old habits from my first round of oral chemo: I am not as responsive to texts and calls, I want to nap more, and when I am really feeling well I only want to do things I feel strongly invested in. My energy is so limited. Cancer is literally the best excuse for me to not do things. I hate using the cancer card but it is back in full effect. My body only has so much energy these days. Please forgive me for being a shitty friend. I am trying my best right now to keep my shit together.
Literally.
Today’s song lyrics of the day are brought to you by Teddy Swims.
“Something’s got a hold of me lately
No, I don’t know myself anymore
Feels like the walls are all closin’ in
And the devil’s knockin’ at my door, whoa”
-
Subscribe
Subscribed
Already have a WordPress.com account? Log in now.